Healthcare Payer Network Management Market Overview
The Healthcare Payer Network Management Market plays a critical role in the efficient operation of modern healthcare systems. It encompasses a set of tools and services that support the organization, administration, and optimization of payer networks — the systems of healthcare providers, insurers, and third-party administrators.
As value-based care models replace traditional fee-for-service frameworks, payers must ensure that their networks are robust, efficient, and transparent. The goal of network management is to create cost-effective, high-quality care partnerships that deliver better patient outcomes while managing reimbursement and compliance effectively.
AI and Innovation in the Healthcare Payer Network Management Market
Artificial Intelligence (AI) is driving transformation in the Healthcare Payer Network Management Market. AI-powered platforms are streamlining provider credentialing, automating claims adjudication, and optimizing contract management. Machine learning algorithms now assist in evaluating provider performance, risk scoring, and fraud detection.
Through real-time data analytics, payers can better match members with suitable providers, monitor network adequacy, and address care gaps. Predictive analytics also allows insurers to anticipate network strain and respond proactively. These innovations reduce administrative burden and significantly enhance operational efficiency, which is critical for managing complex, multi-tiered payer networks.
Future Trends in the Healthcare Payer Network Management Market
The future of the Healthcare Payer Network Management Market is being shaped by several emerging trends. Among them, interoperability across platforms and data systems is key. With regulatory pressure to eliminate data silos, payer networks are increasingly integrating with provider EHRs and patient portals. Additionally, blockchain technology is gaining traction for secure, verifiable provider data exchange.
Digital twins and AI-driven simulations are being explored to optimize network design and test policy impacts. Another notable trend is the rise of hybrid network models that combine narrow networks with concierge and value-based services, offering both efficiency and member satisfaction.
Rising Demand in the Healthcare Payer Network Management Market
Demand in the Healthcare Payer Network Management Market is on the rise due to evolving reimbursement models, increasing healthcare costs, and the need for operational efficiency. Payers are under pressure to reduce administrative overhead while maintaining network adequacy and compliance with state and federal mandates. As patient expectations grow and value-based models become the norm, insurers require better tools to evaluate provider performance, manage utilization, and negotiate contracts.
Additionally, the shift toward telehealth and digital care has expanded the complexity of network management, pushing for more agile and responsive solutions.
Key Market Highlights
-
Surge in AI and analytics integration across network management platforms.
-
Increasing adoption of cloud-based payer solutions.
-
Growth in demand for automated credentialing and contracting tools.
-
Expansion of virtual care provider networks and telehealth inclusion.
-
Enhanced focus on regulatory compliance and interoperability.
Market Growth Drivers
Several factors are fueling the growth of the Healthcare Payer Network Management Market:
-
Value-Based Care Transition: The move toward outcomes-based reimbursement requires better network visibility and performance management.
-
Healthcare Cost Containment: Rising costs drive payers to optimize networks for both quality and efficiency.
-
Regulatory Compliance: Rules such as the No Surprises Act and CMS interoperability mandates require updated network capabilities.
-
Demand for Digital Health Integration: As digital care models grow, networks must expand to include telehealth and remote monitoring providers.
These drivers are accelerating investment in modern network management infrastructure and tools.
Market Restraints
While the market holds great promise, the Healthcare Payer Network Management Market faces several challenges:
-
Data Fragmentation: Disparate data sources and lack of integration create barriers to network visibility.
-
High Implementation Costs: Advanced network management systems can be costly to deploy and maintain.
-
Provider Resistance: Some providers resist network optimization initiatives due to concerns about reimbursement rates and administrative burden.
-
Regulatory Complexity: Constantly changing regulations can make compliance difficult without scalable solutions.
These limitations emphasize the need for flexible and adaptive platforms in the network management ecosystem.
Opportunities in the Market
Opportunities in the Healthcare Payer Network Management Market are substantial:
-
Emerging Technologies: Innovations in AI, blockchain, and API-based architectures offer transformative potential.
-
Expansion into Underserved Markets: Smaller payers and rural health systems represent untapped demand.
-
Value-Based Network Expansion: Building specialized networks for chronic care, behavioral health, and wellness can improve outcomes and lower costs.
-
Partnerships and Ecosystems: Collaborations between tech firms, payers, and providers can create integrated platforms with greater capabilities.
As the industry shifts to a more patient-centered and data-driven model, these opportunities will shape the next phase of network management innovation.
Regional Insights
-
North America dominates the Healthcare Payer Network Management Market, driven by the U.S. healthcare system’s complexity, high insurance penetration, and regulatory frameworks.
-
Europe is seeing steady growth as universal healthcare systems adopt digital transformation strategies for payer-provider interactions.
-
Asia-Pacific is emerging rapidly, particularly in countries like India and China, where health insurance adoption is expanding along with digital infrastructure.
-
Latin America and the Middle East & Africa are slowly integrating network management solutions, driven by private payer initiatives and international investment in digital health.
Also Read@ https://www.pharma-geek.com/dehydration-monitoring-devices-market/
Healthcare Payer Network Management Market Companies
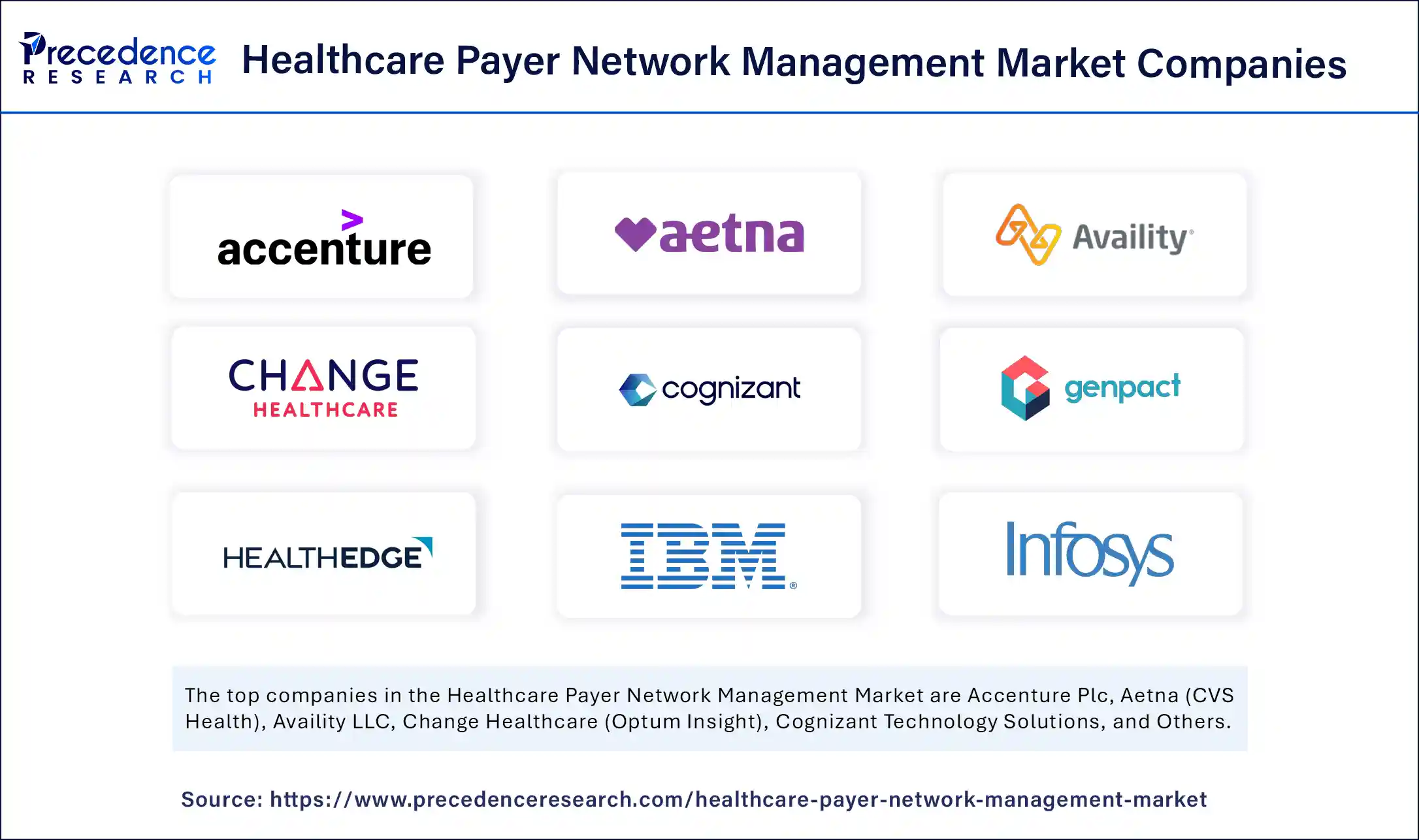
- Accenture Plc
- Aetna (CVS Health)
- Availity LLC
- Change Healthcare (Optum Insight)
- Cognizant Technology Solutions
- Genpact Limited
- HealthEdge Software Inc.
- IBM Corporation
- Infosys Limited
- Inovalon Holdings Inc.
- McKesson Corporation
- Medversant Technologies
- Optum (UnitedHealth Group)
- Oracle Corporation
- SAS Institute Inc.
- Tata Consultancy Services (TCS)
- TriZetto Healthcare Products (Cognizant)
- Verisk Analytics Inc.
- Wipro Limited
- ZeOmega Inc.
Get Free sample Link @ https://www.precedenceresearch.com/sample/6722
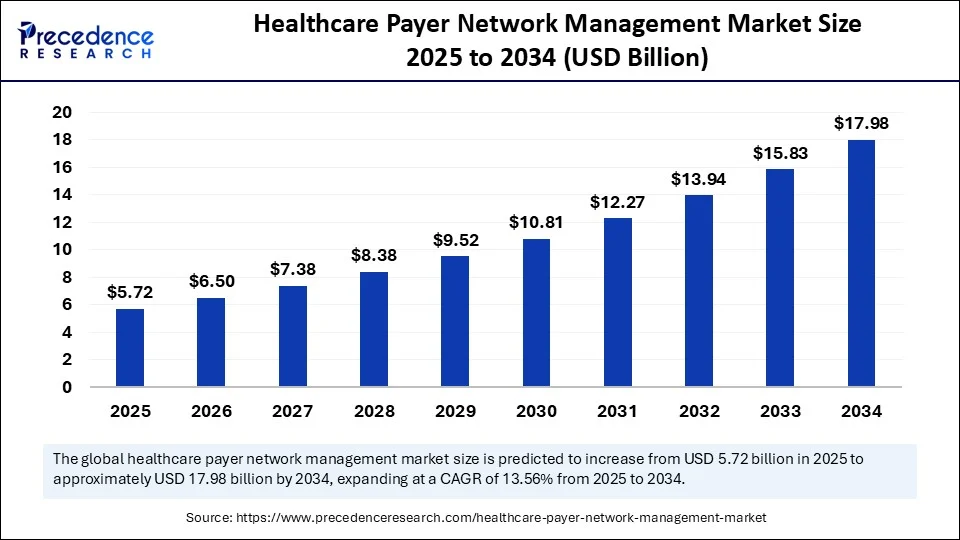
- Healthcare Payer Network Management Market Size to Reach USD 17.98 Billion by 2034 - September 9, 2025
- Protein Characterization and Identification Market Size to Reach USD 8.04 Billion by 2034 - September 9, 2025
- Biopharmaceutical Packaging Market Size to Reach USD 179.66 Billion by 2034 - September 9, 2025
